Improving the Safety of Diagnosis and Therapy in the Inpatient Setting
Background
Ensuring accurate and timely diagnoses and delivering the correct treatment is a significant challenge in acute care. Delayed, missed, or incorrect diagnoses are considered diagnostic errors (DEs), which can lead to improper therapy and harm patients. Even with accurate diagnoses, treatments may not be administered promptly or appropriately.
Study Goals
To address this issue, our AHRQ-funded Patient Safety Learning Laboratory (PSLL) used the Safer Dx framework to create a learning environment to address the problem of DEs in acute care. We rigorously analyzed system and cognitive factors that lead to diagnostic process failures (DPFs) and DEs in the hospital.
Our Approach
Our process began with problem analysis, followed by the design, development, implementation, and evaluation.
During problem analysis, we applied systems engineering methods to characterize DEs and DPFs in general medicine patients. We also validated a structured electronic health record (EHR) chart review process for detecting and analyzing cases, and characterized trigger events.
During the design phase, we used human factors methods to iteratively refine a suite of EHR-integrated interventions targeting common and significant DPFs, such as failure or delay in ordering tests, which were prioritized for development.
During the main trial, we sampled cases from high and low risk patient cohorts before and after implementation to evaluate the impact of this intervention on DE outcomes.
Results
The final intervention included a 5-step diagnostic time-out that clinicians could conduct with the patient; a DE risk dashboard column with configurable parameters to adjust baseline risk estimates in real-time; and a 10-item patient diagnostic questionnaire whose responses were communicated to clinicians.
Based on a stratified sample of 675 cases, we observed a non-significant decrease in DE (primary or secondary diagnoses, harmful or non-harmful) in the post- compared to the pre-implementation period. The intervention trended towards clinically important improvement, especially for high-risk cohorts
Results
The final intervention included:
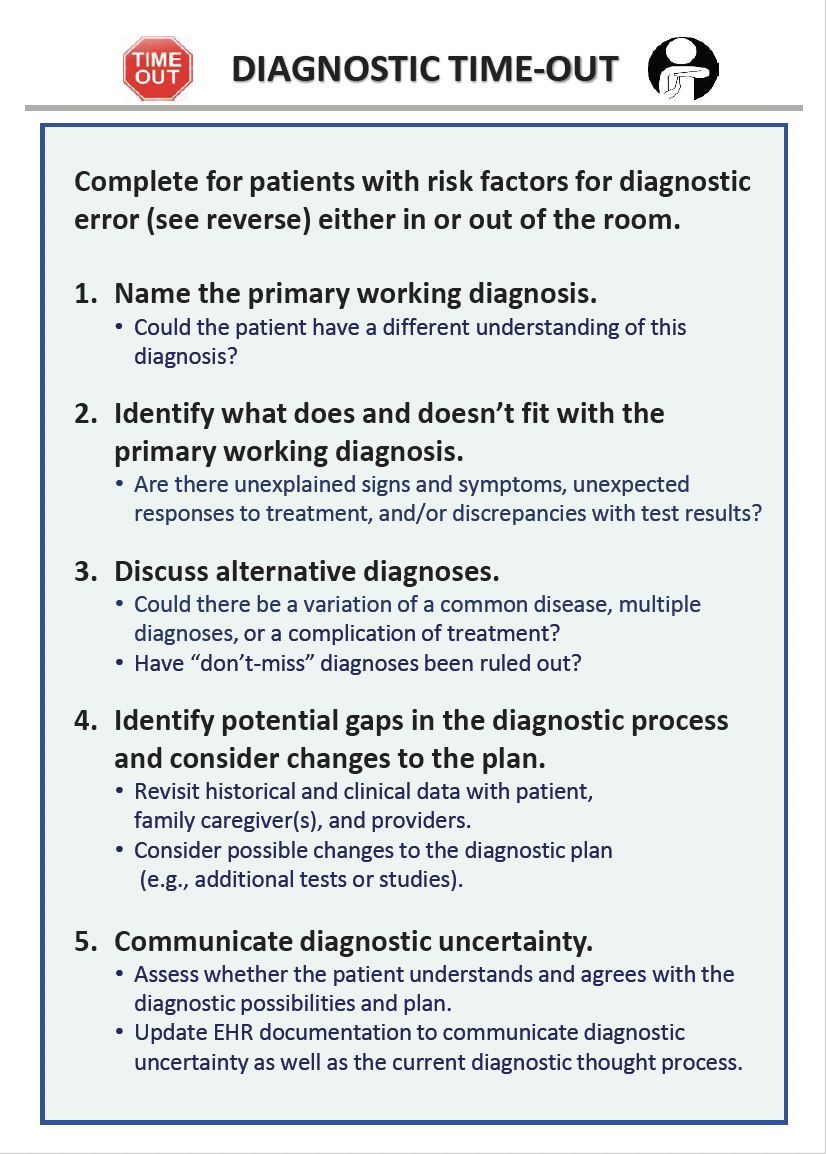
– 5-step diagnostic time-out that clinicians could conduct with the patient;
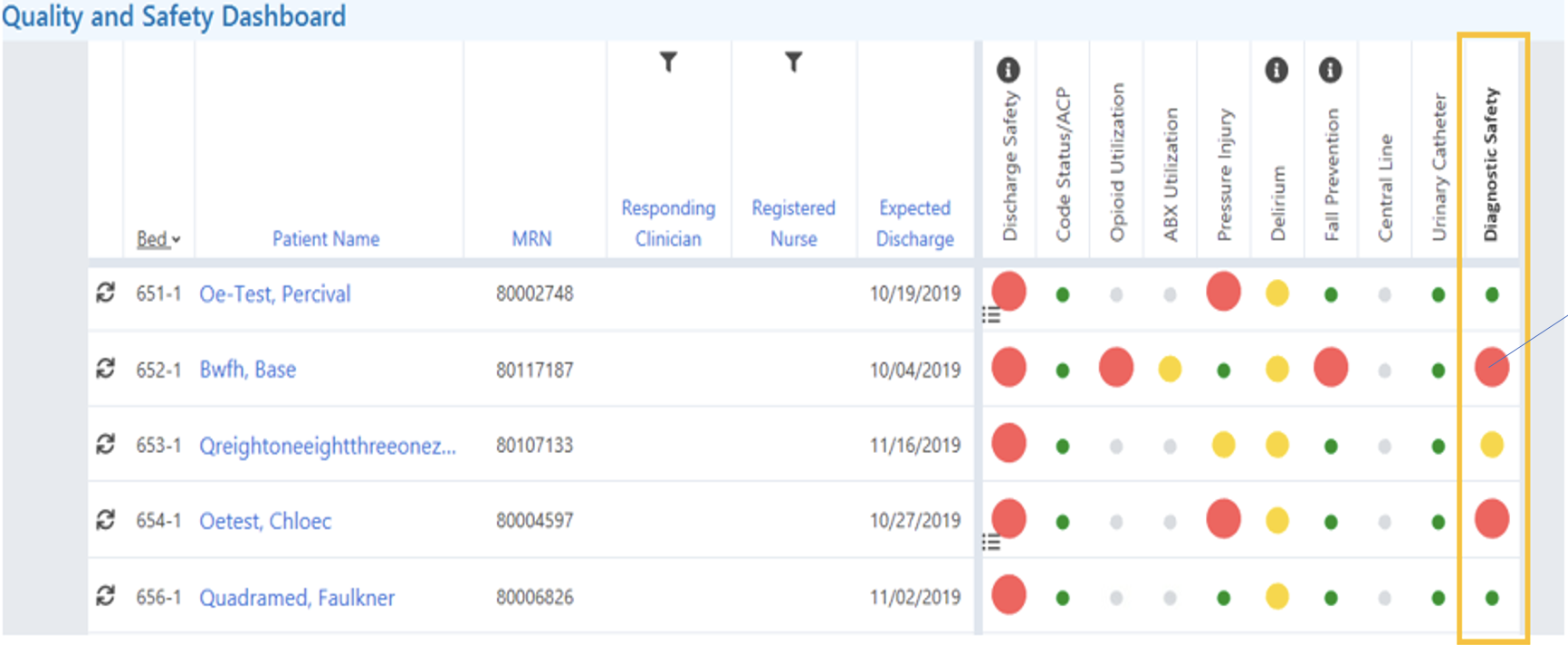
– DE risk dashboard column with configurable parameters to adjust baseline risk estimates in real-time;
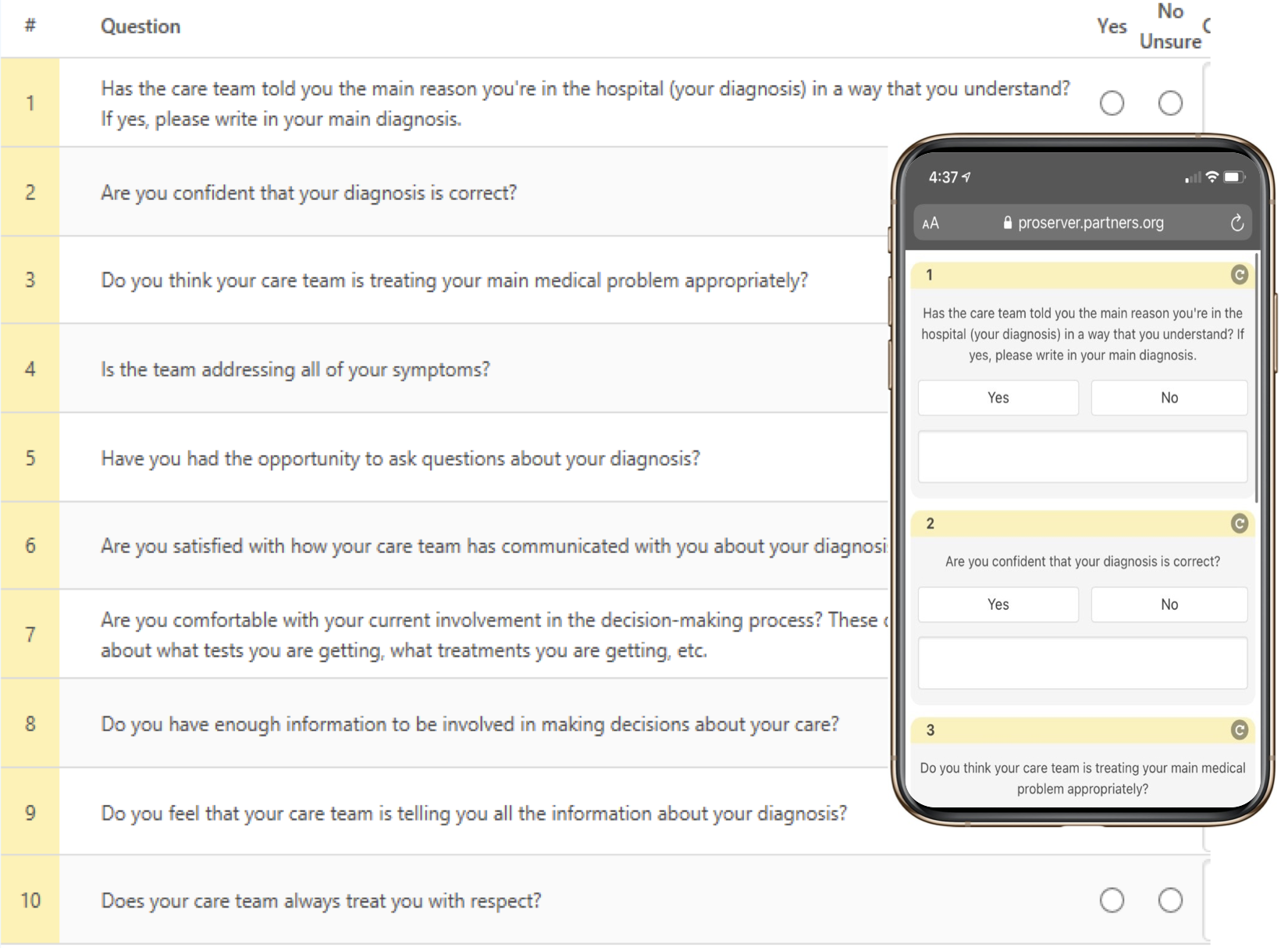
– 10-item patient diagnostic questionnaire whose responses were communicated to clinicians
Based on a stratified sample of 675 cases, we observed a non-significant decrease in DE (primary or secondary diagnoses, harmful or non-harmful) in the post- compared to the pre-implementation period.
The intervention trended towards clinically important improvement, especially for high-risk cohorts.
Diagnostic Time-Out
Diagnostic Error Risk Dashboard Column
Patient Diagnostic Questionnaire