PROSPECT
Promoting Respect and Ongoing Safety Through Patient-centeredness, Engagement, Communication, and Technology
This project was sponsored by the Gordon and Betty Moore Foundation
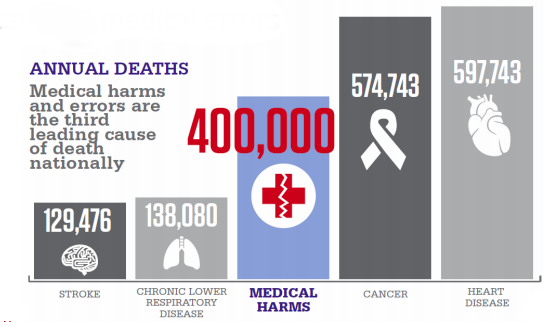
Ineffective care team communication is a leading cause of medical error. The PROSPECT study implemented provider-facing and patient-facing digital health tools to promote team communication and patient activation.
Background & Goals
Transform the intensive care environment through implementation of a patient-centered intervention
Specific Aims
1. Minimize preventable harms
2. Optimize the overall experience of patients (and care partners) by facilitating engagement and promoting dignity and respect.
3. Reduce unnecessary healthcare resource utilization and associated costs.
PROSPECT utilizes baseline data of both team communication and patient activation to create and test care innovations that improve patient and family engagement and reduce preventable harm:
Ineffective healthcare team communication is a leading root cause of medical errors. Team communication challenges include: multiple hand-offs, involvement of numerous professional and paraprofessional providers, varied communication methods, simultaneous parallel conversations, information silos, inconsistent beliefs on patient or family role in the care process, etc.
Patient activation + IT Tools = Patient Engagement
Patient-centered care is respectful and responsive to individual patient preferences, needs, and values. A precondition for patient-centered care is patient engagement. Patient engagement is the combination of patient activation (having the confidence and knowledge necessary to take action in maintaining and improving one’s health) and interventions/tools designed to promote activation and positive health behaviors. Activated, engaged patients are more likely to engage in preventive behavior (check-ups, screenings, etc.), engage in healthy behavior (healthy diet, regular exercise), avoid health-damaging behavior (smoking and illegal drug use), as well as incur less costs.
PROSPECT preliminary work included a collaborative approach to designing and implementing a structured team communication program enabled by health information technology. Methods to generating such tools included interviews, workflow observations, and focus groups. Additionally, a participatory, iterative design of the communication model and a suite of shared documentation and communication tools were utilized. The PROSPECT intervention implemented both “provider-facing” tools and “patient-facing” tools.

Results
Provider-Facing Tools
Tools clinicians can use to encourage care team communication and promote patient safety.
Microblog
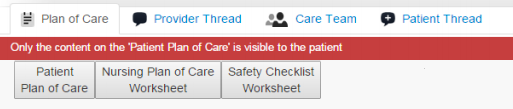
The Web-Based Patient-Centered Toolkit (PCTK) was expanded to include suite of provider-facing tools. A microblog is a communication tool with multiple functionalities. The “Care Team” tab accurately and reliably identifies care team members for a particular patient. The “Patient Thread” encourages patients to proactively engage providers and the “Provider Thread” consolidates the plan of care dialog into a single, transparent conversation thread.
The “Plan of Care” tab is a multidisciplinary plan of care platform that includes the Patient Plan of Care…
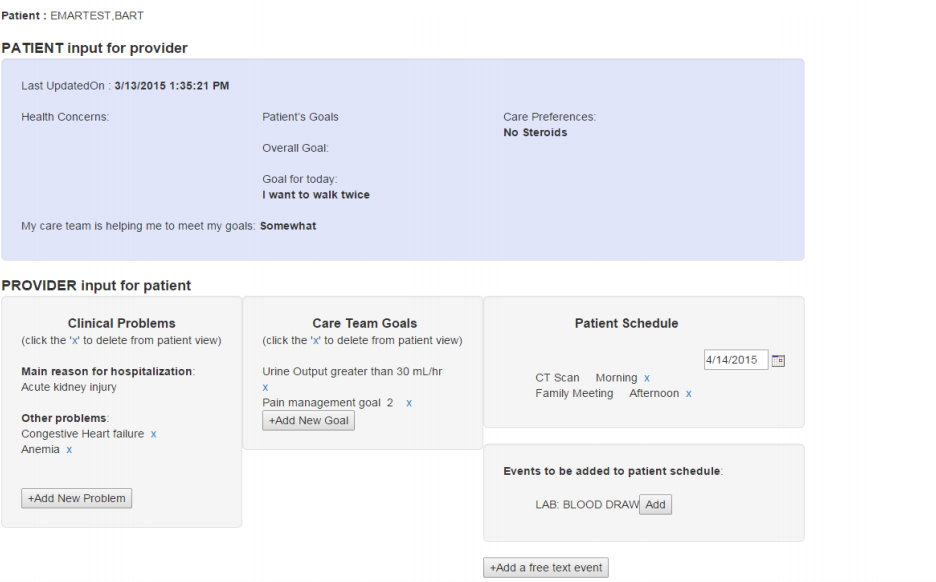
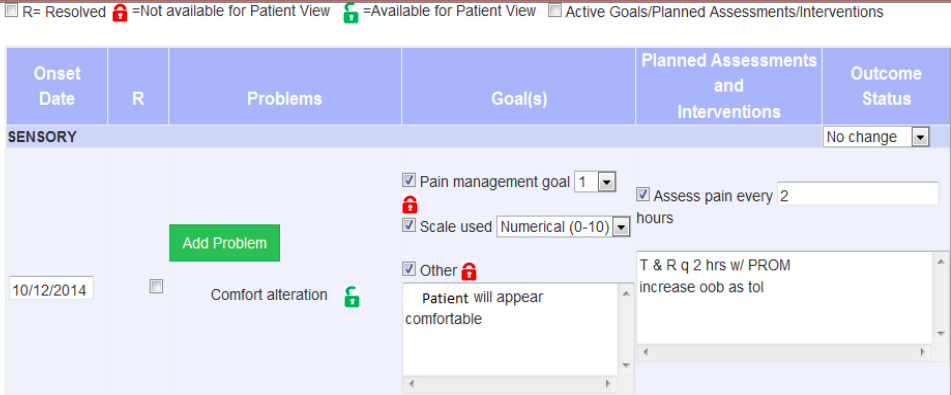
the Nursing Plan of Care Worksheet…
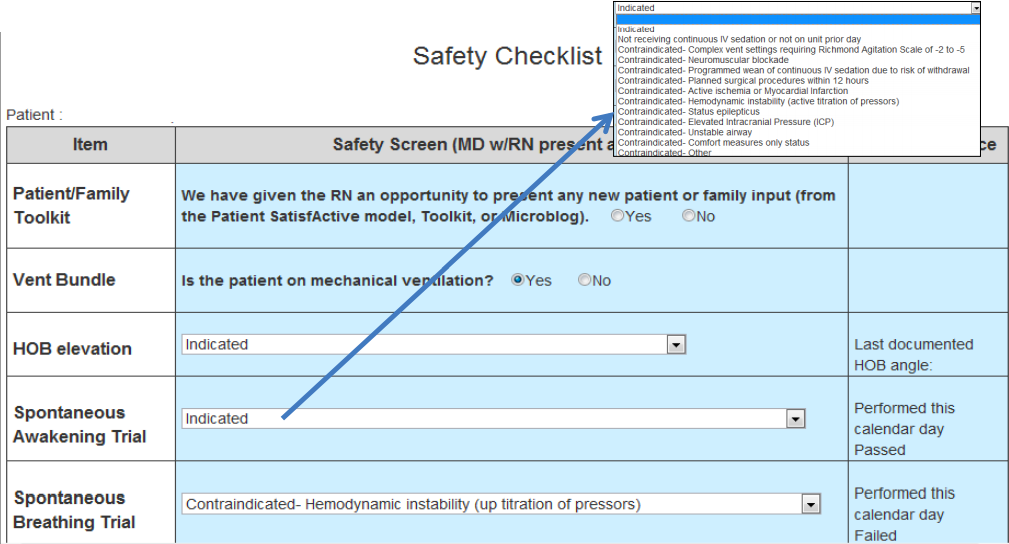
and the Safety Checklist Worksheet.
Patient-Facing Tools
Tools patients can use to actively participate in their plan of care
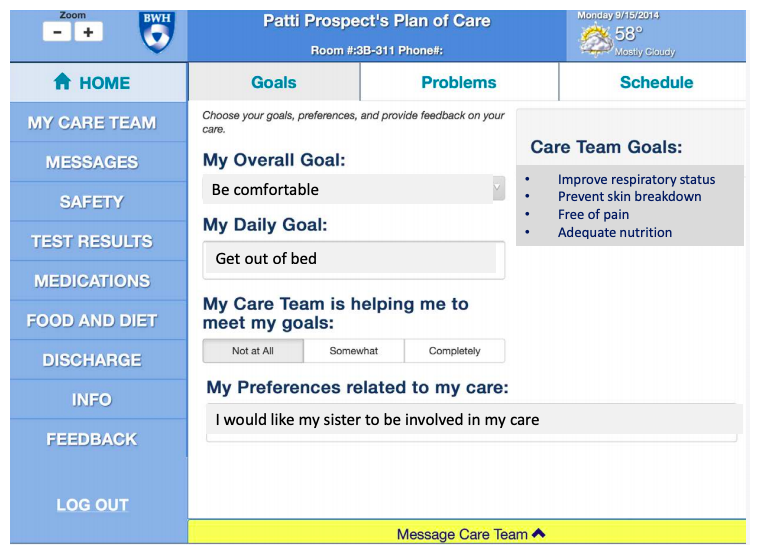
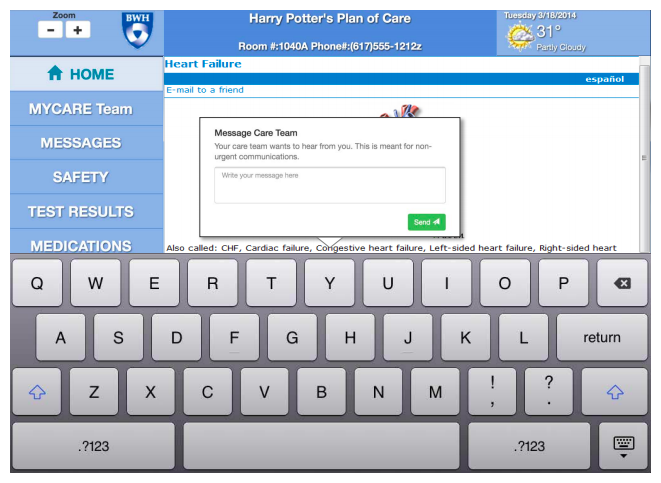
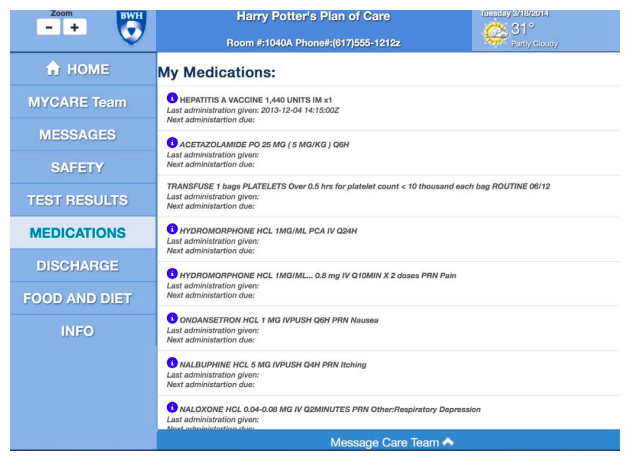
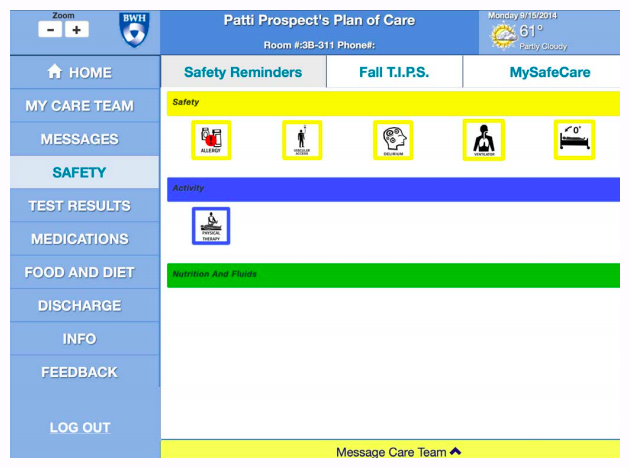
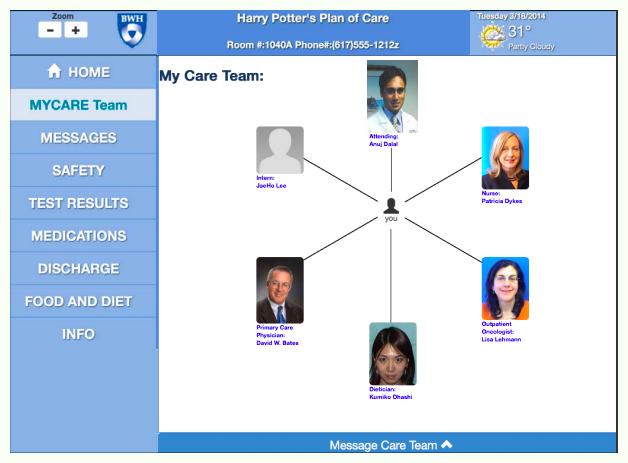
Like the microblog, patient-facing tools have multiple functionalities. One PROSPECT intervention implemented was refining the Patient SatisfActive® Model for use in BWH MICU. Using this tool, patients can set goals and update preferences. Additionally, patients are able to view and message members of their care team, review safety reminders and diet plans, as well as view test results and medications.
Patient SatisfActive® Model
Press the side arrows <> to view different functionalities
Conclusions
- PROSPECT improved relationships with patients and families and reduced the likelihood that they would be harmed in the MICU.
- Recognition of the value of technology and its impact on workflow is essential. Attention to provider “readiness” and workflow is key to success.
- Patient Satisfactive Model was useful for reinforcing patient-centered practices and increasing the collaboration and communication needed for successful adoption of technology. Technology can be useful for engaging patients but additional work is needed to overcome barriers to patient use. Additionally, more work needs to be done to flesh out patient and provider roles in establishing goals of care.
- Technology is ubiquitous in all other aspects of many patients and care partners lives. We need to create tools to engage all stakeholders that support good communication and evidence-based care.