PSLL 2.0 Part 2
Improving the Safety of Diagnosis and Therapy in the Inpatient Setting
We are designing and developing a suite of Electronic Health Record (EHR)-integrated digital health tools to address the high frequency of diagnostic errors in the inpatient setting.
Background & Goals
Problem Analysis
Identify and analyze cases of diagnostic error during hospitalization
Diagnostic errors are complex to study. They are hard to assess, difficult to detect, and have various definitions. We define diagnostic errors as diagnoses that are missed, incorrect, or delayed. We aim to measure diagnostic error rates, validate several “e-triggers”, and identify potential predictors of diagnostic error.
Events captured in the Electronic Health Record (EHR), or “e-triggers”, may be clues that a diagnostic error has occurred. As an example, transfers to the ICU, especially when unexpected, may indicate clinical deterioration of a missed diagnosis.
Some examples of e-triggers

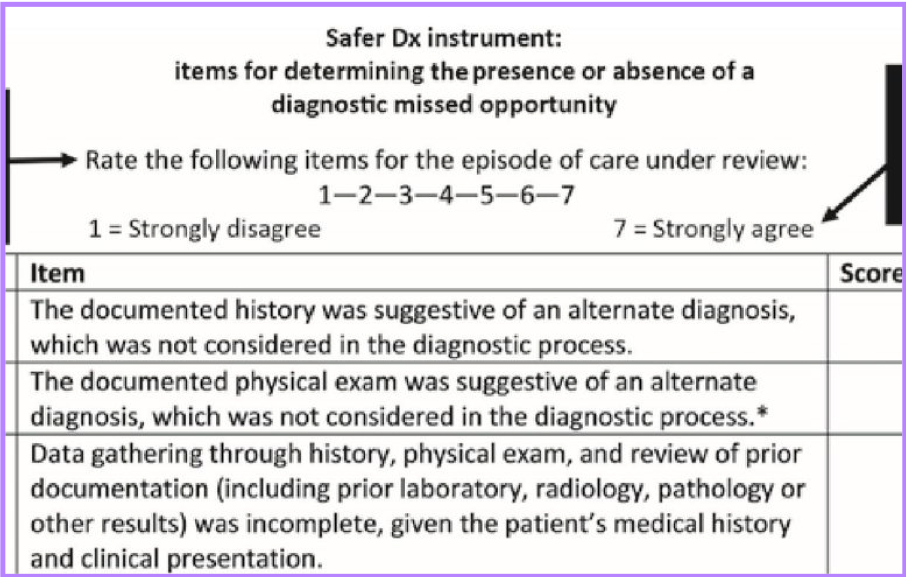
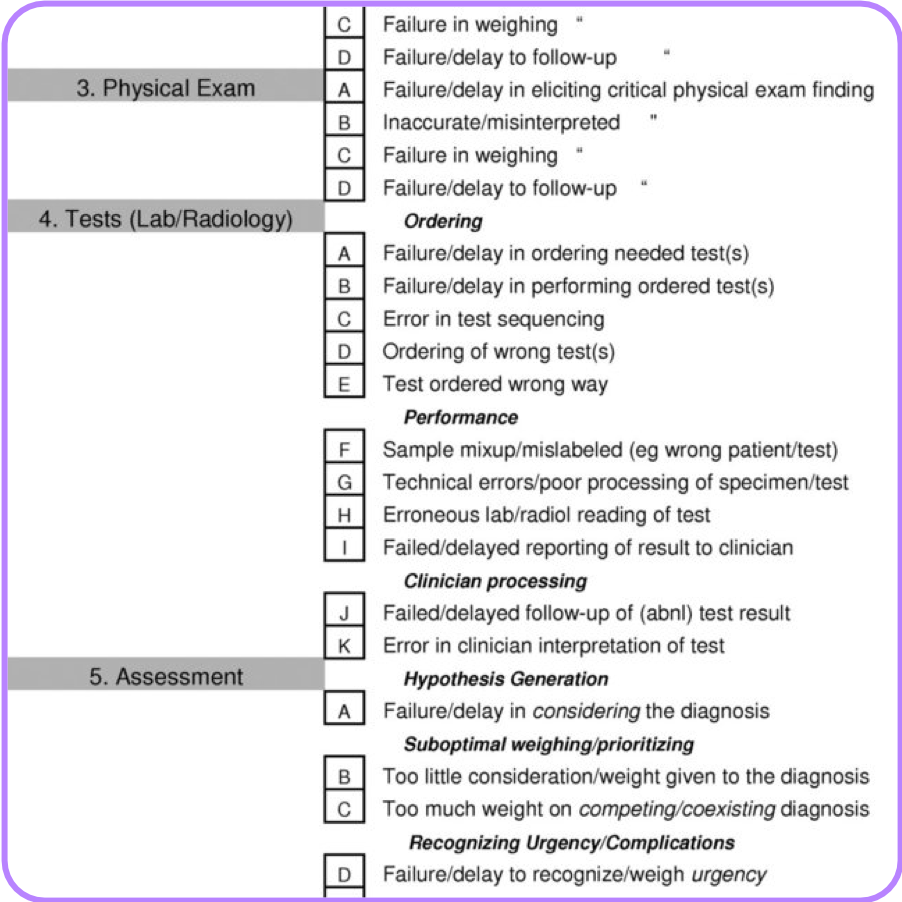
In order to determine if a diagnostic error has occurred, we adapted existing tools to create a chart review tool for the inpatient setting. One tool we adapted was the Safer Dx instrument, a 12 question tool that chart reviewers use to assess the likelihood of diagnostic error. It also provides a score that can help determine a particular case’s risk for diagnostic error. Another tool adapted to the inpatient setting was the Using Diagnostic Error Evaluation and Research (DEER) Taxonomy which classifies specific failure points (e.g., failure to order a test). There are 41 failure points across the 6 diagnostic process dimensions.
Safer Dx Instrument
6 Process Dimensions
DEER Taxonomy
We have trained adjudicators conduct chart reviews to evaluate representative cases and determine instances of errors, preventability of errors, and significant failure points. Click here for an example of a representative case from the past month. Please contact us if you are a physician looking to get involved in our chart reviews!
Fishbone Diagram Template
Systems Engineering approaches such as evaluating care processes and information flow is critical in identifying the causes of diagnostic error. Methods include process mapping, FMEA focus groups, fishbone diagrams, and fault trees.
Results
Intervention Design and Development
Design and develop a set of interventions that mitigate harm due to failures in the diagnostic process.
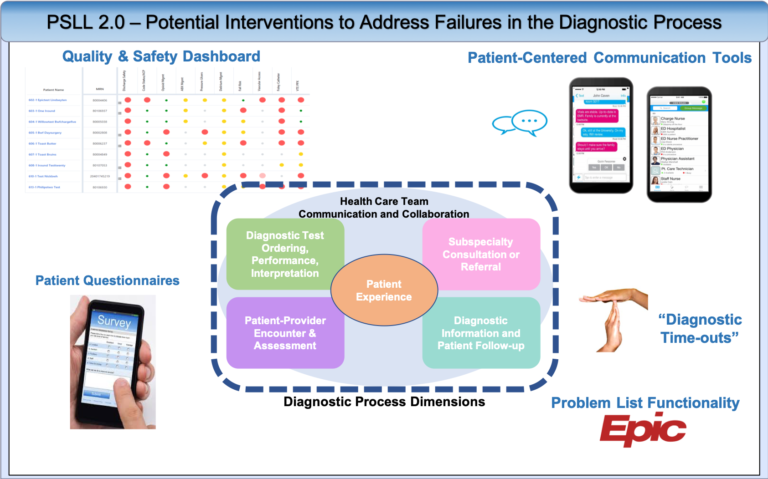
Using a systems engineering, human factors, and data analytic methods, we are designing and developing a suite of EHR-integrated digital health tools to address the high frequency of diagnostic errors in the inpatient setting. Potential solutions will leverage both patient-facing and clinician-facing tools to address the failures in the diagnostic process.
Implementation and Evaluation
Implement the interventions and assess the impact on diagnostic errors that lead to patient harm.
We are currently testing some of our interventions such as our “diagnostic time-out” cards. These cards encourage physicians to reevaluate and reengage with patients who are at risk for diagnostic error. Having a standardized time-out during a time of uncertainty pushes physicians to reexamine potential failures in the diagnostic process such as a breakdown in care team communication or cognitive biases. After 5 rounds of testing and revisions, we finalized the card. We are currently in the process of training physicians and physician assistants to regularly use the diagnostic time-out cards on their patients.
Be sure to watch our example video of how the Diagnostic Time Out plays out in the inpatient setting and download our mobile app below!